Anal Fissures
What are anal fissures?
Anal fissures are a split along the lower part of the anal canal, which is the small area of bowel connecting the rectum with the anus (see figure 1). They are a fairly common condition and it is thought that they affect up to 11% of the population, with both men and women equally affected. This condition generally occurs in people aged between 20 and 40 years old.
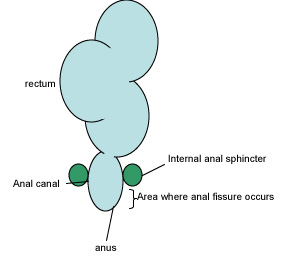
Figure 1. Diagrammatic representation of anal canal and other structures
What causes anal fissures?
There are several theories to the causes of anal fissures. The passage of hard stools and/or constipation are thought to play a role. However, there are other risk factors associated with the cause of anal fissures, and these include childbirth, previous anal surgery, Crohn’s disease and even diarrhoea. Infections such as tuberculosis, HIV and syphilis may also help cause anal fissures.
The mechanism behind the cause of anal fissures is not completely known. However, it is thought that the anal sphincter, which is an area of muscle used to control the passage of stools, plays an important role. Studies have shown that the tone of the internal anal sphincter is higher than normal in patients with anal fissures, and this can lead to a reduced amount of blood getting to the anal canal. This decreased amount of blood may then go on to cause the anal fissure.
However, anal fissures can also be caused by low anal sphincter tone, although this is much less common and is often associated with other diseases such as HIV or diabetes.
What types of anal fissures are there?
Anal fissures are either acute or chronic. Acute fissures occur with a sudden onset and heal within 2 weeks, whereas chronic anal fissures are generally fail to heal within 8 weeks.
Anal fissures can also be defined by location. Most of these are located at the back (known as posteriorly), although they can also be located at the front (anteriorly) or at the sides. Anal fissures can also be located in more than one location. The location may give a clue to the cause of the anal fissure - for example a fissure located at the sides may be more likely due to Crohn’s disease.
What are the signs and symptoms of anal fissures?
Often the story that a patient gives, as well as the examination, are enough to diagnose anal fissures.
Patients usually complain of:
- Sharp stabbing or burning pain that comes on when passing stools. There may be a history of constipation or straining, or patients may be able to trace the onset of pain from one particular incident
- Bleeding, which is bright red and separate from the stool (such as on the tissue)
- Itching around the anus (known as pruritus ani)
- There may be piles
In most patients, simple inspection by parting the buttocks will enable a diagnosis to be made and the fissure to be seen. In other cases, a small telescope may be used to look for fissures or to exclude anything else. This can be done in clinic.
How are anal fissures treated?
Medical treatment
Anal fissures are usually treated with medicines. The patient is advised to reduce constipation by eating high fibre diet and drinking plenty of water. Stool softeners can also be used.
Creams can be applied to the fissure, and these include analgesics, which aim to numb the area and so make it less painful. Other creams, such as glyceryl trinitrate and isosorbide dinatrate, aim to increase the blood flow to the area and reduce anal sphincter tone. Side effects include headaches and a burning sensation to the anus. A different type of drugs (called calcium channel blockers), such as diltiazem or nifedipine are also used, but give similar side effects.
The use of injections of botulinum toxin A into the anal sphincter have also been studied. This paralysis the muscles of the sphincter and so reduces the tone. However, the side effects include temporary incontinence, bleeding and infection. This is therefore not the first line of treatment.
Surgical treatment
If all medical treatment fails, then surgery may offer another route in treating chronic anal fissures. The most common procedure is called a lateral sphincterotomy, where the internal sphincter is operated on. However, there is a risk of the anal fissure recurring and/or incontinence.
Another surgical option is fissurectomy, where the fissure is removed. It has been suggested that using this technique with botulinism injection is effective. Another option could be where an area of skin around the anus is used to cover the fissure.
Main Ref: The Management of Anal Fissure: ACPGBI Position Statement Cross et al. 2008